Infectious Disorders
Zika virus: neurologic complications
Oct. 08, 2024
MedLink®, LLC
3525 Del Mar Heights Rd, Ste 304
San Diego, CA 92130-2122
Toll Free (U.S. + Canada): 800-452-2400
US Number: +1-619-640-4660
Support: service@medlink.com
Editor: editor@medlink.com
ISSN: 2831-9125
Toll Free (U.S. + Canada): 800-452-2400
US Number: +1-619-640-4660
Support: service@medlink.com
Editor: editor@medlink.com
ISSN: 2831-9125
Worddefinition
At vero eos et accusamus et iusto odio dignissimos ducimus qui blanditiis praesentium voluptatum deleniti atque corrupti quos dolores et quas.
Patent foramen ovale is a prevalent congenital cardiac defect, occurring in about 25% of the general population. Although it is generally asymptomatic, studies have found associations between patent foramen ovale with ischemic stroke and migraine. The best management strategy for ischemic stroke in the setting of patent foramen ovale has historically been controversial; however, several randomized controlled trials have bolstered the evidence for device intervention in the secondary prevention of ischemic stroke.
|
• Although often asymptomatic in the general population, patent foramen ovale is associated with two major neurologic conditions: stroke and migraine headache. | |
|
• Direct causality and pathogenic implications of patent foramen ovale in stroke and migraine occurrence remain to be established. | |
|
• The benefit of transcutaneous patent foramen ovale closure for stroke prevention has been demonstrated in several randomized controlled trials including CLOSE, REDUCE, and DEFENSE-PFO. | |
|
• The decision to refer a case for patent foramen ovale closure requires thorough work up to rule out alternate stroke mechanism, as well as eligibility criteria for positive trials. | |
|
• Interdisciplinary conversations between cardiology and neurology should occur prior to recommending patent foramen ovale closure. |
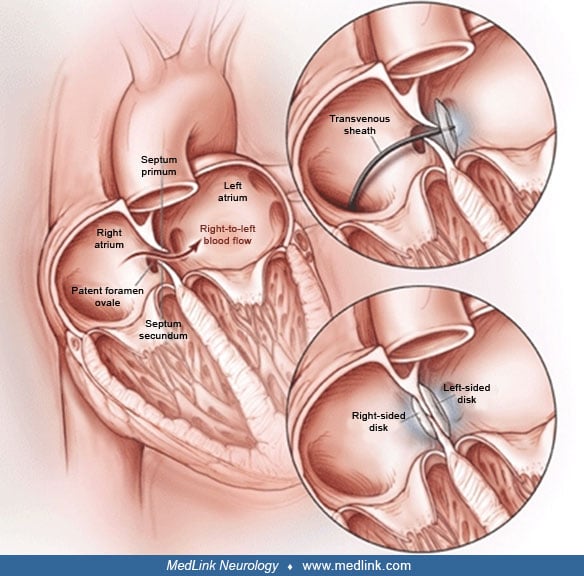
In a significant proportion of the general population, there are various forms of interatrial communication, such as patent foramen ovale, atrial septal defect, and associated disorders such as atrial septal aneurysm. The foramen ovale is a flap valve structure formed by the septum primum and septum secundum in normal fetal cardiac anatomy; patent foramen ovale is the abnormal persistence of this hole into adulthood.
Atrial septal defect is a congenital defect in which an open, interatrial communication, devoid of any tissue flap covering the opening occurs. Patent foramen ovales are differentiated from atrial septal defects as no septal tissue is missing in patent foramen ovale (126). Atrial septal aneurysm, first described in the literature by Silver and Dorsey in 1978, refers to the redundant tissue in the region of the fossa ovalis (117). It is present if the base of the aneurysmal protrusion measures at least 1.5 cm in diameter and there is either a fixed protrusion of the fossa ovalis at least 1 to 1.5 cm into an atrium or phasic excursion of the fossa ovalis throughout the cardio-respiratory cycle exceeding 1.5 cm from the plane of the atrial septum (40; 93).
These disorders, although sharing some purported associations with disease states such as paradoxical embolic phenomena and cryptogenic strokes, are not synonymous and have different associated clinical features, complications, and controversies regarding their management. This article will focus on patent foramen ovales and their relationship to neurologic disease states with a brief mentioning of associated atrial abnormalities such as atrial septal defect and atrial septal aneurysm as they pertain to patent foramen ovales. The importance of patent foramen ovale stems from the fact that the scientific literature is replete with studies that imply a causative or associative role for them in various neurologic disorders. These disorders include strokes caused by paradoxical embolic phenomena, cryptogenic strokes, and transient ischemic attacks as well as migraines with aura, cluster headaches, cerebral autosomal dominant angiopathy with subcortical infarcts and leukoencephalopathy (CADASIL), cryptogenic and recurrent brain abscesses, obstructive sleep apnea, transient global amnesia, paradoxical air embolisms in neurosurgical patients undergoing surgery in the sitting position, neurologic decompression illness, and the presence of “multiple ischemic brain lesions” in divers, and deep white matter and periventricular white matter hyperintensities (on T2/FLAIR MRI sequences) in patients with Alzheimer dementia (71; 33; 65; 66; 28; 04; 98; 02; 53; 106; 70; 09; 91; 35; 60; 129; 104). In the scientific literature, a significant number of studies and expert opinions question these associations and emphasize that these interatrial communications are for the most part innocent bystanders (36; 114; 75; 82; 99). Thus, the relationship of patent foramen ovales to neurologic diseases and the ways to best manage them are controversial issues.
The earliest documentation of paradoxical embolism through a patent foramen ovale is in the 1877 text of Julius Cohnheim followed by the 1880 paper by Moritz Litten (73). In more modern times, a group of investigators based in Paris, France first postulated, in 1988, an important role for patent foramen ovales in young patients (younger than 55 years of age) with cryptogenic stroke based on a case-control study (71).
This common anatomic finding (estimated to occur in approximately 25% of the population) is frequently discovered during the workup for etiology of ischemic stroke, and has been particularly linked to cryptogenic stroke (a stroke that does not have an otherwise identifiable etiology, or has multiple possible etiologies after a thorough workup is conducted). As a 1-way intermittent shunt, it is not associated with any clinical symptoms (such as dyspnea or exercise intolerance) that may be found in other septal defects. There are typically no findings on physical exam to suggest the presence of a patent foramen ovale. Patent foramen ovale incidence declines with increasing age, but size may increase (39).
Other illnesses that have been associated with a patent foramen ovale include platypnea-orthodeoxia syndrome (a rare condition characterized by dyspnea and desaturation in the upright position-platypnea, with improvement in the supine position-orthodeoxia), decompression sickness, obstructive sleep apnea, fat embolism, and tumor embolism (68). A review suggested no link between migraine and patent foramen ovale (121).
As there are no natural history studies on those who have patent foramen ovale, the prognosis is not known. For healthy patients with a patent foramen ovale, annual stroke risk has been estimated as low as 0.1% (74). In general, patients with stroke and patent foramen ovale are not felt to have a higher risk of recurrent cryptogenic stroke or transient ischemic attack, either independently (56) or when compared to those without patent foramen ovale (52). Evidence has additionally suggested an increased risk of perioperative stroke in patients with patent foramen ovale (95). There is likely heterogeneity of risk among patients with patent foramen ovale; a score which examines the degree of causality between patent foramen ovale and cryptogenic stroke (the Risk of Paradoxical Embolism, or RoPE score) can be of use to clinicians (56) and is discussed later in this article.
A 23-year-old woman with no past medical history presented with two-day history of acute onset left facial droop, dysarthria, and increased sleepiness. She was in her usual state of health the night before and woke up with left facial droop and slurred speech. She initially attributed her symptoms to fatigue, but she later presented to the emergency department for further evaluation. She denied any headache or neck pain or recent injury. Her past medical history, surgical history, family history, social history, and review of systems were unrevealing. Her only medication was an oral contraceptive pill that she started taking in the past year. On examination, her blood pressure was 127/65 mm Hg and heart rate was 86 beats per minute. Her general exam was within normal. Neurologic exam was pertinent for impaired short-term memory, left lower facial droop, and mild dysarthria. Labs including metabolic panel, blood counts, and drug screen were within normal limits. She had a computerized tomography scan of the brain showing a right thalamocapsular hypodensity suggestive of a subacute infarct. She subsequently had a magnetic resonance imaging (MRI) of the brain confirm the area of infarction. Vascular imaging with magnetic resonance angiography head and neck with fat suppressed images (dissection protocol) was normal.
Transthoracic echocardiography showed the presence of bubbles in the left atrium after intravenous agitated saline injection, suggestive of a cardiac shunt. Subsequent transesophageal echocardiogram revealed a patent foramen ovale with an atrial septal aneurysm. Hypercoagulable workup was reassuring. Lower extremity venous Dopplers and pelvic magnetic resonance venography showed no deep or pelvic vein thrombosis. She was started on aspirin and taken off the combined oral contraceptive pills. After two years, she remains stroke free and, with the exception of mild difficulty with short-term memory, most of her symptoms from the stroke have resolved.
Patent foramen ovale. In the developing embryonic heart, a series of events enumerated below lead to the development of a foramen ovale starting at the end of the fourth week of gestation (108).
|
• A sickle-shaped crest grows from the roof of the common atrium into the lumen, the first portion of the septum primum; the two limbs of this septum extend towards the endocardial cushions in the atrioventricular canal. | |
|
• The opening between the lower rim of the septum primum and the endocardial cushion is the ostium primum. | |
|
• Subsequent extensions of the superior and inferior endocardial cushions attempt to close the ostium primum. | |
|
• A new crescent-shaped fold, the septum secundum, appears on the right atrial side. This never forms a complete partition. | |
|
• With further growth and fusion with adjacent structures, the free concave edge of the septum secundum begins to overlap the ostium secundum. | |
|
• The opening left by the septum secundum is called the oval foramen or foramen ovale. | |
|
• The upper part of the septum primum gradually disappears, and the remaining part becomes the valve of the oval foramen. | |
|
• The foramen ovale allows the passage of blood (mainly the oxygenated blood from the inferior vena cava) from the right atrium to the left atrium. | |
|
• After birth, when lung circulation begins and left atrial pressure increases, the valve of the oval foramen is pressed against the septum secundum, obliterating the oval foramen, thus, achieving complete separation of the right and left atria. This, however, does not occur in 20% to 25% of the normal population producing the patent foramen ovale. | |
|
• The reason for failure to fuse and obliterate the oval foramen in these people is not known, but some studies have implicated genetic factors (06). | |
|
• In some instances, the oval foramen closes prematurely, in prenatal life, and leads to massive hypertrophy of the right atrium and ventricle with underdevelopment of the left side of the heart. In these cases, death usually occurs shortly after birth. |
Atrial septal aneurysm. Atrial septal aneurysms are occasionally found in patients with patent foramen ovale; prevalence is estimated between 1% to 3% (117; 118). These are saccular formations of the intraatrial septum primum. Eighty-three percent of patients with an atrial septal aneurysm have a concurrent patent foramen ovale (110). To be considered an atrial septal aneurysm, there must be either protrusion of the septum at least 1.5 cm beyond the plan of the atrial septum or phasic excursion during the cardiorespiratory cycle exceeding 1.5 cm and a base of the aneurysmal protrusion that is at least 1.5 cm in diameter (40). Atrial septal aneurysms may bulge into the right or left atrium. Patients with both an atrial septal aneurysm and patent foramen ovale may have a higher risk of stroke than when either occurs in isolation or when neither is present (77).
Patent foramen ovale and stroke. The relationship between patent foramen ovale and stroke, particularly cryptogenic stroke, is an area of continued interest. To review, cryptogenic strokes are those with no clear etiology revealed after standard workup, and account for between 20% to 30% of all stroke etiologies (43). These are frequently felt to be embolic in nature, specifically embolic strokes of undetermined source. Embolic strokes tend to have maximal neurologic deficit at onset with rapid improvement due to disruption or lysis of embolic material with distal embolization into smaller end arteries.
Cerebral embolism may occur due to passage of a venous thrombus to the left atrium through the patent foramen ovale. This requires reversal of the normal pressure gradient to allow right atrial pressure to exceed left atrial pressure, which occurs with pulmonary hypertension and several other normal and disease states. In healthy subjects, right to left shunt may only occur during times of transiently increased intrathoracic pressure, such as with coughing or during the Valsalva maneuver. Stroke attributed to passage of a thrombus across a patent foramen ovale is more likely a single cortical infarction or multiple small scattered lesions, and occurs more frequently in the vertebrobasilar circulation (62). Predilection for the vertebrobasilar circulation may relate to increased blood flow during the Valsalva maneuver (45; 61). Search for a venous source of embolus may be unrevealing (36). This has been attributed to delay in imaging, complete thrombus migration, inability to detect residual thrombi, or undetected thrombus in a calf or pelvic vein. One trial found that cryptogenic stroke had increased prevalence of pelvic deep venous thrombosis (21), suggesting that such evaluations should be undertaken in patients with cryptogenic stroke.
Some suggest that there are features of patent foramen ovale that directly relate to paradoxical emboli. Severe right-to-left-shunt, right-to-left shunt at baseline, a larger opening of the patent foramen ovale, and high membrane mobility may place patients at greater risk for recurrent embolism (46; 27). A second possible mechanism implicates atrial septal aneurysm, if present, as a potential nidus for clot formation (111). Others suggest that propensity to clotting in the setting of hereditary or acquired thrombophilia increases the risk of stroke in the setting of a patent foramen ovale (49).
There is a new tool to help clinicians determine whether a cryptogenic stroke may be related to a patent foramen ovale or whether the patent foramen ovale represents an incidental finding. The RoPE score (Risk of Paradoxical Embolism) derives from a master database constructed using 12 component databases from large observational studies. This RoPE database contains information on over 3600 patients with cryptogenic stroke who underwent investigation into the presence of a patent foramen ovale. Points are assigned for absence of traditional risk factors and for age, with higher points for younger patients. The higher the point score, the more likely the stroke was related to patent foramen ovale, and, conversely, the less likely the patient was to experience a recurrent stroke within two years (56).
Patent foramen ovale and silent brain infarcts. Silent brain infarcts are generally defined as hyperintensities on T2-weighted MRI of 3 mm or greater. Although by definition they lack clinically-overt symptoms, silent brain infarcts have been shown to be associated with an increased risk of subsequent stroke, as well as mild cognitive impairment and dementia, independent of traditional vascular risk factors (125; 26). Silent brain infarcts are traditionally thought to be caused by microangiopathy but can also be caused by microembolism, especially when located outside deep brain structures. However, the relationship between patent foramen ovale and silent brain infarcts remains unclear, with conflicting data from several observational studies.
In one prospective cohort study assessing the rate of both clinically-apparent and clinically-silent brain infarcts in patients with pulmonary embolism both with and without patent foramen ovale, the frequency of silent brain infarcts was found to be significantly higher in patients with patent foramen ovale (19). A larger study that analyzed the relationship of silent brain infarcts and paradoxical embolism through patent foramen ovale found that over 50% of healthy adult patients with silent brain infarcts specifically located outside of perforating artery territory had right-to-left cardiac shunts, suggesting an association (61). However, another prospective study that followed over 1000 asymptomatic individuals both with and without patent foramen ovale for a median of 11 years found no association between the presence of patent foramen ovale and the accumulation of silent brain infarcts (32).
Thus far, patent foramen ovale closure has not been shown to prevent silent brain infarcts. The GORE-REDUCE Trial, discussed in detail later, randomized patients with patent foramen ovale and cryptogenic stroke to patent foramen ovale closure with antiplatelet therapy or to antiplatelet therapy alone (119). Although the incidence of new brain infarcts was found to be significantly lower in the closure group than the medical therapy group, the incidence of silent brain infarcts did not differ between the two. In an analysis of REDUCE trial (84), after two years of follow up, patients who underwent closure of patent foramen ovale experienced lesser clinical stroke orf silent infarcts on MRI (4.7%), as compared to patients who only had medical therapy (10.7%) (RR 0.44 [95% CI, 0.24 – 0.81], p = 0.02). Clinical strokes were less common in closure patients compared with medically treated patients (1.3% vs. 5.8%, p=0.001), whereas silent MRI infarcts were similar (3.4% vs. 4%, p= 0.81).
It is unknown whether patent foramen ovale closure reduces the risk of subsequent stroke in patients with silent brain infarcts. At the time of this writing, there is no evidence to suggest that patent foramen ovale closure is beneficial in such patients.
Patent foramen ovale and migraine. The second most commonly studied neurologic disease associated with patent foramen ovale is migraine with aura. Although patent foramen ovale has been thought to be more common in patients who suffer migraine or migraine with aura (101; 118), several studies including a cross-sectional population-based cohort have not found this to be the case (107; 38; 17).
Migraine has also been associated with silent brain infarcts, but several studies have found no clear mediating effect of patent foramen ovale on this association (13; 50).
An autopsy study of normal hearts found an overall incidence of patent foramen ovale of 27% (39). Age and size did not differ by gender. As age increased, prevalence decreased, from 34.3% in the first three decades of life to 25.4% during the fourth through eighth decades and 20.2% during the ninth and tenth decades. Most patients (98%) had a foramen ovale less than 10 mm in diameter. Size increased with increasing age, with a mean of 3.4 mm in the first decade and 5.8 mm in the tenth decade. A population-based study (Stroke Prevention: Assessment of Risk in a Community, or SPARC) found the prevalence of patent foramen ovale to be 25.6% (83), with no change in prevalence by age group.
Detection of a patent foramen ovale in a normal or healthy individual does not warrant a discussion of further treatment such as percutaneous closure. Prevention of other associated conditions such as decompression illness may be found in separate clinical summaries addressing these conditions.
Retrospective, case-control studies have suggested a direct role of the patent foramen ovale in occurrence of cryptogenic stroke, particularly in patients younger than 55 years of age (98; 80). However, these studies have significant methodologic concerns, including the possibility of ascertainment bias (lack of blinded echocardiogram interpretation) and control subjects with potential underdetection of patent foramen ovale (due to a variety of referral reasons which may lead to limited investigation into presence or absence of a patent foramen ovale).
There have been three prospective studies examining patent foramen ovale and recurrent stroke risk; these all explored whether closure of the patent foramen ovale reduced the risk of recurrent stroke in patients with cryptogenic stroke. The first trial, CLOSURE I (37), investigated the use of the STARFlex Septal Closure System; subsequent trials used the Amplatzer PFO Occluder device (RESPECT) (15; 81). All three of these trials failed to show in their primary analysis a benefit of patent foramen ovale closure for prevention of cryptogenic embolism in adults with prior cryptogenic stroke. Current practice guidelines reflect these findings, stating “clinicians should not routinely offer percutaneous PFO closure to patients with cryptogenic ischemic stroke outside of a research setting” (85).
These trials have been analyzed in great detail to determine if there is a subgroup that may benefit from closure of the patent foramen ovale, with at least six metaanalyses thus far. The first metaanalysis did not find benefit of patent foramen ovale closure over medical therapy using unselected devices, although it did note that select devices may be superior (without increasing the risk of atrial fibrillation), warranting further trials (96). RESPECT suggested that highly selected patients with cortical infarcts and no vascular risk factors may benefit from closure (37); a presentation of 10-year followup from this trial shows potential benefit in patients with true cryptogenic stroke (122), although full results have not been released and followup at 10 years shows significant attrition with unequal groups. An analysis suggests that closure reduces risk of recurrent stroke in adjusted but not unadjusted analysis (55). An additional trial looking at use of the GORE HELEX Septal Occluder for prevention of recurrent stroke has completed enrollment, with results pending and anticipated in the near future (ClinicalTrials.gov).
When evaluating a patient for paradoxical embolism, the echocardiographer will need to distinguish between a patent foramen ovale, a coexisting atrial septal aneurysm, an atrial septal defect, and a pulmonary arteriovenous malformation (which is typically suggested by the presence of a late right-to-left shunt). In addition to paradoxical emboli from the venous system, other potential cardiac or extracardiac sources of emboli, such as benign cardiac tumors (myxoma and papillary fibroelastoma) valvular strands, and aortic arch thrombosis must be considered when evaluating patients with cerebrovascular embolism or cryptogenic stroke.
Patent foramen ovale is most commonly found during investigation of the heart done for a variety of indications including stroke, syncope, presence of a murmur, or ischemic heart disease. Transthoracic echocardiography and transesophageal echocardiography are the most frequent modalities used to diagnose a patent foramen ovale, but transcranial Doppler and magnetic resonance imaging of the heart have also been used. An intravenous contrast agent is given during the strain phase of the Valsalva maneuver to diagnose right to left shunting.
Transesophageal echocardiography is superior to transthoracic echocardiography in diagnosis and determination of morphology of patent foramen ovale (112). For those patients with suspected paradoxical embolism or cryptogenic stroke, this is most commonly felt to be the definitive imaging procedure of choice. As an invasive procedure requiring cooperation and sedation, transesophageal echocardiography does have potential for complications, including bronchospasm, hypoxia, arrhythmia, upper gastrointestinal trauma, or bleeding; these occur in approximately 0.2% of patients (24). In patients that are high risk for this procedure, transcranial Doppler is a reasonable alternative. A metaanalysis found that transcranial Doppler is a reliable noninvasive test, with sensitivity of 97% and specificity of 93% for detecting intracardiac right-to-left shunt (89).
Given the wide prevalence of patent foramen ovale and the very weak association with stroke risk in population-based studies, the vast majority of patent foramen ovale are thought to be incidental and do not require medical treatment. Controversy about treatment options becomes an issue when a patent foramen ovale is detected in the setting of ischemic stroke or migraine with aura.
Recommendations from neurologic and cardiovascular societies such as the American Academy of Neurology and the American College of Cardiology suggest withholding antithrombotic agents with isolated patent foramen ovale in the absence of other indications for antithrombotic therapy (85). This is because given the extremely low stroke risk in patients with patent foramen ovale (0.1% per year) (74), it is unlikely that the benefit of these agents would outweigh the bleeding complication risk. In addition, there are no studies demonstrating the efficacy of patent foramen ovale closure in asymptomatic patients. On the contrary, a large retrospective study showed that routine closure of septal defects such as patent foramen ovale and atrial septal defect in patients undergoing cardiothoracic surgery was associated with a higher risk of perioperative stroke (adjusted odds ratio 2.47 95%, CI 1.02-6.0) when compared to patients with septal defects not intervened upon (69). Due to the lack of supporting evidence and potential for complications, as with thrombotic therapy, routine closure of asymptomatic patent foramen ovale is not recommended.
The management of patients with patent foramen ovale in the setting of an ischemic stroke remains controversial. The treatment options include medical treatment with antiplatelet agents or anticoagulation therapy versus patent foramen ovale occlusion. Given the high prevalence of patent foramen ovale in the general population, it is of paramount importance to determine whether the patent foramen ovale is likely to be causative of the event versus incidental.
General measures. It is standard care to provide all available risk reduction strategies to patients with an ischemic stroke or transient ischemic attack. These include blood pressure reduction as well as the use of statins and antiplatelet therapy (86). In addition, certain general measures may be beneficial for patients at risk for paradoxical embolism. They include avoidance of Valsalva maneuver-mimicking activities, thus preventing right-to-left shunting of blood across the atrial septal communication; avoidance of prolonged sitting (in long airplane or other journeys); sitting with knees flexed and legs dependent; and crossing the legs when sitting and passive standing (86).
Medical options.
Antiplatelet vs. anticoagulation treatment. There are several studies with mixed results with regards to the best antithrombotic agent for secondary stroke prevention in patients with ischemic stroke in the setting of a patent foramen ovale. A retrospective study of 90 patients and a metaanalysis found warfarin therapy to be superior to aspirin (22; 97). These results have been deemed inconclusive as these studies were not blinded, had multiple end points, had treatment assignments at the discretion of the consulting neurologist, and had frequent crossovers (64). These were followed by the PICSS study, which did not demonstrate a statistically significant difference between aspirin and warfarin on the risk of subsequent stroke or death among patients with cryptogenic stroke and a patent foramen ovale (48; 70; 86). Because the PICCS study was not limited to patients with cryptogenic stroke, it does not adequately answer the question of whether anticoagulation therapy is superior to antiplatelet therapy in patients with cryptogenic stroke and patent foramen ovale. More importantly, because patent foramen ovale is fairly common in the general population, it is of importance to determine whether the patent foramen ovale is the likely mechanism of the index event as opposed to an incidental finding. Investigators designed the Risk of Paradoxical Embolism (RoPE) score based on a cohort of patients from multiple prospective population-based studies to address this question. Results from this cohort demonstrated that in patients with a cryptogenic stroke and a patent foramen ovale, a RoPE score of six or more implies the high likelihood of the patent foramen ovale being causative versus incidental whereas in patients with RoPE scores of less than 6, the patent foramen ovale is likely to be incidental (56). Interestingly, additional analysis from the same patient cohort showed that the risk of recurrent stroke in patients with the highest RoPE scorer (9 or 10) was up to 2% over two years, supporting previous evidence that the overall risk of recurrent stroke attributed to the patent foramen ovale is low regardless of the treatment modality (56). In patients whose patent foramen ovale was thought to be incidental based on the RoPE score, anticoagulation treatment was associated with a lower risk of stroke recurrence at two years whereas in patients whose patent foramen ovale was thought to be causative of the index event, there was no difference between the two treatment modalities (122). Moreover, an individual patient metaanalysis that included 2385 patients with 227 composite endpoints (stroke/transient ischemic attack/death) showed no significant benefit of anticoagulation when compared to antiplatelet therapy (adjusted HR 0.76, 95% CI 0.44-1.27) (54).
In patients with patent foramen ovale and cryptogenic stroke, it is critically important to complete a thorough stroke work up for alternative mechanism rather than assuming that the patent foramen ovale is the culprit. This is especially relevant in older patients with lower RoPE scores where other mechanisms such as paroxysmal occult atrial fibrillation or atrial mechanisms might be at play.
The NAVIGATE-ESUS trial studied rivaroxaban versus antiplatelet therapy alone for patients with embolic stroke of undetermined source (ESUS) and was negative for the primary outcome (44). In patients with a patent foramen ovale and embolic stroke of undetermined source, anticoagulation was associated with lower risk of recurrence (HR 0.54, 95% CI 0.22-1.36) but with increased risk of major hemorrhage (HR 2.05, 95% CI 0.51-8.18), and when these data were pooled with the PICCS and CLOSE trials, the benefit of anticoagulation in secondary stroke prevention achieved statistical significance (HR 0.48, 95% CI 0.24-0.96, p=0.04) (51). Data from the RESPECT-ESUS trial, however, showed no significant benefit of dabigatran over aspirin in patients with patent foramen ovale in secondary stroke prevention (HR 0.88, 95% CI 0.45-1.71) (31). Moreover, updating the metaanalysis mentioned above with these data from RESPECT-ESUS resulted in no statistically significant benefit of anticoagulation as compared to antiplatelet therapy for recurrent stroke (OR 0.70, 95% CI 0.43-1.14) (30).
Therefore, in the absence of an indication for anticoagulation therapy, antiplatelet therapy appears to be the antithrombotic of choice in patients with patent foramen ovale.
Surgical options. Surgical options to close a patent foramen ovale have been offered to patients with patent foramen ovale and a history of stroke, especially when certain high-risk factors are present. These include the Valsalva maneuver preceding the event; hypercoagulable states; multiple strokes or events; and patent foramen ovale characteristics such as large opening (3.4 to 5.8 mm), large right-to-left shunting, right-to-left shunting at rest, presence of an atrial septal aneurysm, high mobility of the valve of the patent foramen ovale, and a well-formed eustachian valve (134; 86). In addition, patients younger than 50 years of age, those with recurrent neurologic events, those with failure of anticoagulation to prevent events, and those intolerant of anticoagulation and at high risk of deep vein thrombosis or pulmonary embolism are considered closure candidates (134).
Three surgical options for closure are available: (1) the traditional open thoracotomy foraminal closure, (2) minimally invasive surgery, and (3) percutaneous closure techniques (64). For open thoracotomy, the rates of postoperative stroke were found to range from 0% to 3.5% in different studies (29; 47; 25). Mortality associated with the procedure was less than 1.5%, and perioperative risks included atrial fibrillation, pericardial sequelae, and the need for re-exploration due to bleeding (29; 47; 94; 25).
Percutaneous device closure is performed by accessing a large systemic vein (usually femoral) and deploying a closure device at the atrial septal communication (patent foramen ovale or secundum atrial septal defect) by means of a catheter.
It is touted as an effective, safe, and commonly employed alternative to surgical closure in patients with patent foramen ovale (130). An alternative to percutaneous closure with devices is the transcatheter closure of patent foramen ovale using radiofrequency energy. The safety and feasibility of this technique was reported (116).
The United States Food and Drug Administration approved two patent foramen ovale occluder devices (the Amplatzer(r) Septal Occluder and the CardioSEAL(r) Septal Occlusion System) under a humanitarian device exemption for the treatment of patients with recurrent cryptogenic stroke due to presumed paradoxical embolism through a patent foramen ovale and who had failed drug therapy (86).
The CardioSEAL(r) devices have undergone two subsequent modifications and were made available as the STARFlex(r) device and, subsequently, as the BioSTAR(r) device. However, soon after the FDA withdrew the humanitarian device exemption approval after finding that the eligible population in the United States described by the approval indication was significantly greater than the 4000 patient per year limit permitted by the humanitarian device exemption (124). The Gore Cardioform Septal Occluder is also FDA-approved for percutaneous patent foramen ovale closure.
Several retrospective studies also suggested that patent foramen ovale closure might reduce embolic events (11; 133; 120). A series of prospective case-control studies looking into outcomes during long-term follow-up after percutaneous closure of patent foramen ovales also demonstrated a lower incidence of recurrent strokes and transient ischemic attacks (16; 42; 128). In a study the cumulative rate of thromboembolic-free survival rate was estimated at 99% in patients younger than 55 and 84% in patients older than 55 years of age (18). However, they constitute relatively weak evidence and are insufficient to establish whether or not device closure of patent foramen ovale is beneficial. Experts, therefore, recommend that all eligible patients be strongly encouraged to enroll in ongoing randomized trials in order to determine the effectiveness of this therapy (86; 123). For patients with patent foramen ovale and atrial septal aneurysm, compared to those with patent foramen ovale alone, percutaneous device closure was shown to have the same efficacy and complication rates (127). For those patients with atrial septal defect and large left-to-right shunt, there is less controversy regarding need for closure to prevent the development of right heart failure (86). Percutaneous device closure can result in major complications (death, hemorrhage requiring transfusion, cardiac tamponade, need for surgical intervention, or fatal pulmonary emboli) with 1.5% incidence; minor complications in 7.9% of cases are also possible (bleeding not requiring transfusion, atrial arrhythmias, device embolization, device thrombosis, air embolism, and allergy to device components) (59).
And yet, strokes occur after the closure of a patent foramen ovale. Persistent residual shunt (especially in those patients with a redundant atrial septum or an atrial septal aneurysm) (136) or a right-to-left shunt in an anatomically distinct site may allow continued paradoxical embolism. An Italian patent foramen ovale closure study reported a high rate of residual shunt at 6 and 12 months’ follow-up (19.5% and 18%, respectively); however, the associated rate of recurrent neurologic event was low (2.25% at 6 months and 0.8% at 12 months), suggesting that closure was a safe procedure (14). Thrombus may spontaneously form on the left atrial wall of the patent foramen ovale; there is an increased risk for atrial arrhythmias in these patients; and finally, patent foramen ovale may not be etiologically linked to recurrent strokes (12; 10; 132; 76; 05; 127; 86).
The RESPECT study randomized patients between 18 and 60 years of age with cryptogenic strokes within 270 days of stroke onset to medical treatment (n=481) versus closure with AMPLATZER (tm) (n=499), and these were followed for a median of 2.1 years from randomization. In the intention to treat analysis, the event rate was lower in the closure arm than in the medical arm (0.61% vs. 1.25% per patient-year) but this did not achieve statistical significance (15). An updated follow-up of patients enrolled in RESPECT was published in September 2017 (109). Nine hundred eighty patients were followed up for a median of 5.9 years. There was a higher dropout rate in the trial in the medical-group versus the patent foramen ovale closure group. In this extended follow-up period, there was a hazard ratio of 0.55 (CI 0.31-0.999, p=0.046) in the patent foramen ovale closure group (for the primary end point representing a composite of recurrent ischemic stroke or death). For the isolated end point of recurrent ischemic stroke of undetermined cause, the hazard ratio for the patent foramen ovale-closure group was 0.38 (95% CI 0.18-0.79, p=0.007).
The PC Trial randomized 414 patients to medical treatment versus closure with AMPLATZER and followed them for a median of 4.1 years. This trial also did not show a significant benefit of closure when compared to medical treatment (HR 0.63; 95% CI, 0.24-1.62; P=.34) (81).
The CLOSURE trial, on the other hand, randomized 909 patients to closure with the STARFlex (CardioSEAL, NMT Medical, Boston, MA) device versus medical therapy and followed them for two years. The cumulative incidence of the composite of stroke or transient ischemic attack was 5.5% in the device-closure group and 6.8% in the medically treated arm (adjusted HR, 0.78; 95% CI, 0.45-1.35; P=.37) (37). An observation that many of the recurrent events were not caused by paradoxical embolism but instead by alternative causes further clouds the results of this trial.
The GORE-REDUCE trial (GORE® HELEX® Septal Occluder/GORE® CARDIOFORM Septal Occluder and Antiplatelet Medical Management for Reduction of Recurrent Stroke or Imaging-confirmed TIA in Patients with Patent Foramen Ovale [PFO] - The Gore REDUCE clinical study) investigated patent foramen ovale closure with a septal occlusion device in parallel with antiplatelet therapy compared with antiplatelet therapy alone (119). Six hundred and sixty-four patients were enrolled and assigned to patent foramen ovale closure versus medical therapy alone in a 2 to 1 ratio. There was a median follow-up of 3.2 years, with recurrent stroke in 1.4% of those in the patent foramen ovale closure group versus 5.4% of patients in the medial therapy group (HR of 0.23, CI 0.29-0.91). Serious adverse events did not differ between the two groups (23.1% in the patent foramen ovale-closure group vs. 27.8% of patients in the medical therapy group), though device-related complications occurred in 1.4% of patients in the patent foramen ovale-closure group. Additionally, approximately 6% of patients in the patent foramen ovale-closure group developed atrial fibrillation.
The CLOSE trial (Closure of Patent Foramen Ovale or Anticoagulants Versus Antiplatelet Therapy to Prevent Stroke Recurrence) examined patients with cryptogenic stroke and high-risk features of their patent foramen ovale (large interatrial shunt or associated interatrial septal aneurysm) (78). Patients were randomly assigned to one of three groups: (1) percutaneous patent foramen ovale closure with antiplatelet therapy, (2) antiplatelet therapy alone, or (3) anticoagulation alone. The primary end point in this trial was recurrent stroke. Six hundred and sixty-three patients were randomized in this trial with a mean follow up of 5.3 years. In this trial, no patients in the group randomized to patent foramen ovale closure had a stroke (0 out of 238 patients). By contrast, 14 out of 235 patients in the antiplatelet therapy alone group had a stroke with a HR of 0.03 (95% CI of 0.0-0.26, p< 0.001). Also, 1.6% of patients in the anticoagulation group suffered a stroke during the study follow-up period. Like in the GORE-REDUCE trial, the rate of atrial fibrillation was increased in the device-closure group (4.6% vs. 0.9%).
The DEFENSE-PFO trial randomized patients with cryptogenic stroke to percutaneous patent foramen ovale closure with medical therapy compared with medical therapy alone (72). Like in the CLOSE trial, they selected patients on the basis of high-risk features of the patent foramen ovale, including the presence of an interatrial septal aneurysm and large patent foramen ovale. The primary endpoint of DEFENSE-PFO was stroke, death attributed to vascular causes, and major bleeding. Additionally, they used the hypermobility observed on transesophageal echocardiography as an additional indicator of a “high-risk” patent foramen ovale. One hundred twenty patients were enrolled in the trial with 60 patients included in each group. Of the 60 patients, 12.9% of patients in the medical therapy alone group suffered the primary endpoint compared with 0 patients in the patent foramen ovale closure group. Two patients (3%) developed atrial fibrillation.
The early trials of patent foramen ovale closure suggested a benefit to device closure of patent foramen ovale in the setting of cryptogenic stroke, but the benefit did not attain statistical significance, leading to uncertainty for patients and practicing physicians. The six major trials of patent foramen ovale closure studied 3560 patients and confirmed the initially observed signal of benefit to device closure. The three most recent trials (GORE-REDUCE, CLOSE, and DEFENSE-PFO) also mandated antiplatelet therapy in addition to device closure. There was evidence of superiority with double disc devices (eg, AMPLATZER or ASOC) compared with alternative designs (110). Ninety-three percent to 96% of patients with double-disc devices had successful technical outcomes versus 87% of patients undergoing closure with umbrella-clamshell devices (110).
A systematic review and network metaanalysis was reported by Mir and colleagues and incorporated 10 randomized controlled trials in total addressing patent foramen ovale closure and medical therapy (including antiplatelet therapy and anticoagulation) (87). This metaanalysis confirmed a risk reduction in recurrent stroke for patients with patent foramen ovale closure versus anticoagulation (risk difference of -87 per 1000 patients per 5-year period). There was a smaller magnitude of difference in the risk of recurrent stroke in patients who underwent device closure of patent foramen ovale when compared with anticoagulation; however, those patients undergoing anticoagulation had a higher risk of bleeding. The authors of this metaanalysis concluded that in patients below the age of 60, patent foramen ovale closure reduces the risk of recurrent stroke when compared with antiplatelet therapy but not when compared with anticoagulation (low certainty conclusion), though anticoagulation increases the risk of major bleeding.
In patients older than 60 years of age with a cryptogenic ischemic stroke and a patent foramen ovale, the patent foramen ovale may be incidental, and the ischemic stroke is more likely to be due to another mechanism such as atrial fibrillation or atherosclerosis of the cerebrovasculature of aortic arch. That said, paradoxical embolism phenomenon may also be more common in the elderly population due to increasing risk of deep vein thrombosis and pulmonary embolism with older age. In older patients, observational data suggest a link between patent foramen ovale and embolic stroke of undetermined source and an association between patent foramen ovale and increased stroke risk (20; 79). Two studies are under way to assess the role of patent foramen ovale in older patients with a stroke or transient ischemic attack (NCT00859885) as well as the interrelation of patent foramen ovale and atrial fibrillation in older people (NCT04285918). Thus at this time, the benefit of patent foramen ovale closure in patients above 60 years old remains uncertain, and the long-term risks of closure are unknown. More studies are needed to evaluate benefits of patent foramen ovale closure in this sub-population that was excluded from the more recent patent foramen ovale trials showing a benefit from patent foramen ovale closure.
Because the RoPE score helps predict the probability of the patent foramen ovale being the etiology of an otherwise cryptogenic ischemic stroke, rather than being an incidental finding, the benefit of patent foramen ovale closure was stratified by the ROPE score. In an individual patient level data metaanalysis of the trials PC, CLOSURE-I, and RESPECT, the benefit of patent foramen ovale closure was demonstrated in patients whose ROPE score was 7 or greater (HR 0.31 95% 0.11-0.85, p = 0.02) as opposed to those with RoPE score less than 7 (HR 0.82 95% CI 0.41-1.59, p = 0.56) (P for interaction = 0.12) (58). Furthermore, a metaanalysis combining all six patent foramen ovale closure trials showed that the benefit of patent foramen ovale closure was more pronounced in patients with high RoPE scores (adjusted HR 0.21 95% CI 0.11-0.42) as opposed to low RoPE score (adjusted HR 0.61 95% CI 0.37-1.00) (P for interaction = 0.02) (57). Therefore, when considering patent foramen ovale closure in a patient with a cryptogenic ischemic stroke, it is crucial to factor whether the patent foramen ovale is incidental or pathogenic.
The benefit of patent foramen ovale closure in patients with small or no right to left shunting remains uncertain. Exploratory analyses of existing trial data suggest that patent foramen ovale closure may not be efficacious in patients with very small shunts (01). Furthermore, patent foramen ovale trials showing a benefit from patent foramen ovale closure excluded patients with small or no right to left shunt. A meta-analysis of all six patent foramen ovale closure trials showed that the benefit of patent foramen ovale closure was more pronounced in patients with substantial shunt size (HR 0.15 95% CI 0.07-0.33) as opposed to those without a substantial shunt size (HR 0.68 95% CI 0.42-1.09) (P for interaction 0.002) (57). Thus, the benefit of patent foramen ovale closure in patients with cryptogenic ischemic stroke and a patent foramen ovale with small shunt remains uncertain, and more studies are needed to test the benefit of patent foramen ovale closure in this patient population.
A metaanalysis of all six patent foramen ovale closure randomized controlled trials examined the association between the RoPE score when added to patent foramen ovale biomarkers (shunt size, presence of atrial septal aneurysm) with benefits of patent foramen ovale closure (57). This metaanalysis introduced the new scoring system, PASCAL (PFO-associated Stroke Causal Likelihood), which combined the RoPE score with patent foramen ovale functional and structural features, namely shunt size and presence of atrial septal aneurysm, in order to further classify the causal relatedness as unlikely, possible and probable (57). Furthermore, patients classified as unlikely using the PASCAL Classification System had no benefit from patent foramen ovale closure (HR 1.14 95% CI, 0.53-2.46), but patients classified as possible and probable had a benefit from patent foramen ovale closure (HR 0.38 95% CI, 0.22-0.65) and (HR 0.10 95% CI, 0.03-0.35), respectively (P for interaction = 0.003). Furthermore, adverse events such as atrial fibrillation beyond day 45 after randomization were higher in the unlikely PASCAL category (4.41%) as opposed to the possible PASCAL category (1.53%) and probably PASCAL category (0.65%). Thus, the PASCAL classification system may help identify patients who are likely to benefit from patent foramen ovale closure and less likely to have device-associated complications (57).
|
• Due to high prevalence of patent foramen ovale, in patients with patent foramen ovale and cryptogenic stroke, clinicians should consider looking for an alternate stroke mechanism. | |
|
• After a thorough diagnostic evaluation excluding other causes such as paroxysmal occult atrial fibrillation (with at least 30 days of continuous cardiac rhythm monitoring), in patients without an indication for anticoagulation therapy, we suggest treatment with antiplatelet agents for most patients with patent foramen ovale and cryptogenic stroke. | |
|
• In general, secondary stroke prevention strategies including statin therapy as indicated, antithrombotic agents, and stroke risk factor modification should be initiated in all patients with patent foramen ovale and ischemic stroke. | |
|
• Anticoagulation remains a treatment option for patients with patent foramen ovale and documented deep venous thrombosis. | |
|
• Closure of a patent foramen ovale should be considered for patients meeting eligibility criteria for the positive trials and in whom a competing mechanism is excluded. The risks and benefits should be discussed thoroughly with the patient before referring them for patent foramen ovale closure. | |
|
• There should be close liaison between a neurologist and cardiologist in selecting patients who are appropriate for patent foramen ovale closure. |
In addition to the usual treatment of migraine with abortive and preventive therapies, based on a series of retrospective, nonrandomized studies, and case-control studies, some authors propose that percutaneous closure of a right-to-left shunt (patent foramen ovale, atrial septal defect, and pulmonary arteriovenous malformation) results in a significant reduction in the prevalence of migraine and migraine with aura (04; 03; 131; 90; 115; 07; 92; 105; 100; 63). However, the problems with study design and lack of long-term follow-up precludes one from drawing definitive conclusions on this treatment modality. Moreover, some authors propose that the use of antiplatelet agents or anticoagulants might play a role in the decreased frequency of migraine after percutaneous closure (100). Countering that hypothesis, however, is the observation that closure of pulmonary arteriovenous malformations by embolization also decreased the frequency of migraine without the use of any antiplatelet agents (102). Paradoxically, some case reports document an aggravation of migraine headache after percutaneous closure (135; 92).
The MIST trial was a prospective, double-blind, randomized, controlled, multicenter trial to evaluate patent foramen ovale closure with the STARFlex(r) device in patients with frequent migraine with aura refractory to two types of preventive medication and without a prior stroke or transient ischemic attack (34). Published data from this trial showed no difference at six months between patent foramen ovale closure and sham treatment for the primary endpoint of headache cure, which was achieved in each group by three patients. Two other trials are in the works, the PREMIUM trial and the MIST II trial (MIST 2006; 103). The PREMIUM trial is a prospective, randomized, sham-controlled, double-blind, multicenter study to evaluate safety and efficacy of the AMPLATZER(r) PFO Occluder and standard of care medical treatment compared to standard of care medical treatment only. It seeks to enroll 466 patients, aged 18 to 55 years with migraine, with or without aura, at 35 sites around the United States (103). The MIST II trial, a prospective, randomized, sham-controlled, double blind, multicenter study to evaluate safety and efficacy of the BioSTAR(r) Bioabsorbable Septal Occlusion Device, is currently underway. A retrospective cohort study of 150 patients with migraines and patent foramen ovale demonstrated that percutaneous patent foramen ovale closure resulted in a high rate of migraine improvement, particularly in migraine with aura but not exclusively (34% of patients became headache free, and 48% experienced significant improvement). Prospective studies assessing the effect of patent foramen ovale closure on migraine headache are underway.
In light of the above observations from the MIST trial and pending completion of the MIST II and the PREMIUM trial, percutaneous closure of a patent foramen ovale or atrial septal defect is not recommended at this time to treat migraine.
At least two case reports seek to attribute paradoxical embolism through a patent foramen ovale in pregnant or postpartum patients as the cause of stroke and recurrent stroke, and one of them has demonstrated safety and efficacy of percutaneous closure of the patent foramen ovale (67; 23). However, as with the association of strokes in nonpregnant patients and patent foramen ovale, this association in pregnant patients is not evidence of causality pending large-scale prospective randomized controlled studies, which probably will never be feasible in pregnant patients considering the rarity of strokes in this cohort. The successful use of intracardiac echocardiography during percutaneous closure, in order to minimize fetal radiation exposure, has been reported in three pregnant patients who had a patent foramen ovale closed for paradoxical embolization related strokes (113).
In general, there are no major management recommendations for anesthetic interventions in the presence of a patent foramen ovale. One unique circumstance is that the operative team must consider avoiding the seated position for neurosurgical patients with a patent foramen ovale to help minimize paradoxical air embolism (35). This study advocates screening for the presence of a patent foramen ovale in patients scheduled to undergo surgery in the sitting position.
All contributors' financial relationships have been reviewed and mitigated to ensure that this and every other article is free from commercial bias.
Shadi Yaghi MD
Dr. Yaghi of NYU Langone Brooklyn has no relevant financial relationships to disclose.
See ProfileMaheen Rana MD
Dr. Rana of Alpert Medical School of Brown University had no relevant financial relationships to disclose.
See Profile
Steven R Levine MD
Dr. Levine of the SUNY Health Science Center at Brooklyn has no relevant financial relationships to disclose.
See ProfileNearly 3,000 illustrations, including video clips of neurologic disorders.
Every article is reviewed by our esteemed Editorial Board for accuracy and currency.
Full spectrum of neurology in 1,200 comprehensive articles.
Listen to MedLink on the go with Audio versions of each article.
MedLink®, LLC
3525 Del Mar Heights Rd, Ste 304
San Diego, CA 92130-2122
Toll Free (U.S. + Canada): 800-452-2400
US Number: +1-619-640-4660
Support: service@medlink.com
Editor: editor@medlink.com
ISSN: 2831-9125
Infectious Disorders
Oct. 08, 2024
Neuro-Oncology
Sep. 25, 2024
Developmental Malformations
Sep. 22, 2024
Stroke & Vascular Disorders
Sep. 12, 2024
Infectious Disorders
Aug. 27, 2024
Neuro-Oncology
Aug. 15, 2024
General Child Neurology
Aug. 14, 2024
Neuro-Oncology
Aug. 14, 2024