Epilepsy & Seizures
Sleep hyperkinetic (hypermotor) epilepsy
Jul. 19, 2024
MedLink®, LLC
3525 Del Mar Heights Rd, Ste 304
San Diego, CA 92130-2122
Toll Free (U.S. + Canada): 800-452-2400
US Number: +1-619-640-4660
Support: service@medlink.com
Editor: editor@medlink.com
ISSN: 2831-9125
Toll Free (U.S. + Canada): 800-452-2400
US Number: +1-619-640-4660
Support: service@medlink.com
Editor: editor@medlink.com
ISSN: 2831-9125
Worddefinition
At vero eos et accusamus et iusto odio dignissimos ducimus qui blanditiis praesentium voluptatum deleniti atque corrupti quos dolores et quas.
This article describes the basics of aphasic seizures. An aphasic seizure is an inhibitory form of epileptic seizure that disrupts cognitive tasks involving language. Transient ischemic attacks or stroke could be first evoked by clinicians not aware of this possibility. Careful examination, medical history, and EEG should help the neurologist in making the correct diagnosis and introducing adequate therapeutics. Aphasia can occur in patients with epilepsy with auditory features and other epilepsies with seizures arising from or spreading to the dominant lateral temporal neocortex.
• Aphasic seizure is a specific type of inhibitory seizure. | |
• Aphasic status epilepticus should be considered in patients with transient and sustained aphasia not better explained by acute acquired brain lesion (stroke). | |
• EEG and brain imaging (including functional brain imaging) could help differentiate an aphasic seizure from aphasia due to other causes. |
Although the functional anatomy of speech processing has been investigated intensively for almost 150 years, the neural organization of speech perception remains highly debated, even in gross anatomical terms (27). Aphasia could be defined as language impairment caused by a permanent or transient injury to the brain, in a previously normal language user. The deficit may range from very limited problems in exact word finding to more pervasive deficits impacting on all language modalities. Speech production, verbal comprehension, word finding, and repetition can be affected to varying degrees, with or without reading and writing abnormalities.
In most left-handed people and almost all right-handers, left hemispheric dysfunction is responsible for language disorders. However, right hemisphere lesions or transient impairment could produce some language problems such as dysprosody. After Paul Brocas description of the loss of articulate speech following ischemic damage located in the posterior inferior frontal gyrus of the left hemisphere, several other aphasia syndromes have been described, including anomic aphasia, global aphasia, transcortical motor aphasia, Wernicke aphasia, conduction aphasia, and transcortical sensory aphasia. Each aphasic syndrome is presumed to be associated with specific brain area damage, although this remains controversial, even with respect to very ancient observations, as in Broca aphasia (24).
As already mentioned on what should be considered as a true aphasic seizure, there are numerous potential causes for a patients inability to speak, and thus, aphasia is not synonymous with not speaking. A comatose patient or a patient refusing to communicate with doctors or caregivers is not aphasic. Evidence of inappropriate use of language should be collected by examiners to document the diagnosis of aphasia: inability to correctly name objects or point to objects named by others, incorrect comprehension or repetition of sentences, words, and non-words, disturbed syntax or grammar, paraphasic errors, etc.
The possibility that aphasia can be the isolated manifestation of an ictal discharge was suspected more than 50 years ago (03; 05). It has been shown that aphasia, as an ictal or postictal phenomenon, is observed in about 17% of patients with focal seizures with impaired awareness (31; 21). In most of these cases, other symptoms accompany or precede the aphasia. Cases where aphasia is the sole ictal symptom or long-lasting aphasia of epileptic origin, as in aphasic status epilepticus, could present a challenging diagnosis (51; 33).
Difficulties in early case reports on the distinction between ictal and postictal aphasia have been pointed out by Rosenbaum and colleagues (53), who were the first to propose diagnostic criteria, which were further revised by Grimes and Guberman (23): (1) the patient must have language production during the seizures (or, at least, attempts to verbally communicate), (2) language production must show aphasic features, (3) consciousness must be preserved, (4) the seizures must be correlated with the aphasia, as documented by EEG monitoring and behavioral testing, (5) the aphasia should resolve, or nearly resolve, concurrent with successful treatment of the seizures. These criteria have been used in subsequent studies (62) and appear to be robust, although they have not been prospectively evaluated in a non-selected population of patients. Further additional criteria may be useful, such as the description after the seizure, by the patient himself, of experiencing difficulties in finding words or word comprehension ictally. It could be emphasized that aphasic seizures should not be accompanied by amnesia of the ictal subjective experience, due to the lack of loss of contact, making the patient unable to report on his failing attempts at speech.
Some aphasic seizures are reported to be triggered by language activities (28). However, and understandably, ictal language disturbances could only be detected when language is currently being used. More than a reflex factor, language should be considered as a revealing factor for aphasic seizures. In a case report, inner speech was reported as potentially involved during aphasic seizures (65). The patient reported spontaneous inner jargon during her seizure.
Numerous papers have cited aphasia as a revealing and isolated symptom of nonconvulsive status epilepticus (35; 60; 66; 23; 16; 10; 46; 45; 58). Motor aphasia as well as sensory aphasia have been reported, depending on the site of the discharge (35). Aphasic status epilepticus represents a diagnostic challenge because the patient may present with rapid-onset isolated aphasia (26; 17; 10; 45), without clinical evidence supporting an epileptic origin, thus, leading doctors to favor stroke as the cause for aphasia.
This consideration has led some authors to consider aphasic status epilepticus as a specific form of inhibitory status epilepticus mimicking transient ischemic attacks or stroke (20; 04; 14). The opportunity to record EEG during the aphasic states often makes the diagnosis possible (14), although EEG can be normal in some rare cases (18). It could be emphasized that in these cases and others, beside EEG, brain imaging remains relevant in providing arguments excluding other causes such as stroke or brain tumor (49; 62; 18). Brain DWI MRI abnormalities could also be of some help for diagnosis, as exemplified in eight patients with aphasic status epilepticus (62). In a study of four patients without EEG abnormalities but with FDG-PET focal hypermetabolism, aphasic symptoms reverted with antiseizure medication (18).
Some case reports of interest could be presented in more detail: A woman with non-fluent aphasia and brief conjugate eye deviation to the right was diagnosed with de novo aphasic status epilepticus (23). Antiseizure medications proved to be efficacious in improving aphasia. Interestingly, the aphasic status epilepticus was related to a small embolic infarction in the territory of the angular branch of the left middle cerebral artery, as evidenced by CT scan. Without video-EEG recording of recurrent aphasic seizures, the seizures might have been left untreated, and aphasia would have been considered the definitive complication of the brain tissue infarction. In reviewing the literature on aphasic status epilepticus, Grimes and Guberman (23) showed that Broca aphasia (13; 26; 52; 17; 53; 66), mixed aphasia (17; 53; 48; 60; 23), and Wernicke aphasia (35; 34; 52) could be almost equally observed, and that, in most cases, the epileptic nature of the aphasia was suspected on clinical history (previous epilepsy). In a study of nine patients with aphasic status, Ericson and colleagues showed that only one patient previously had aphasic seizures, and all patients suffered from left-hemisphere lesions (19). All aphasias were mixed, including expressive and receptive components. In contrast to previous reports, it was underscored that in five patients, no previous epilepsy was evidenced, making the diagnosis of aphasic status difficult (19).
However, in older reports, the diagnosis did not rely on video-EEG recordings, and some cases showed an inconstant response to antiseizure medications, suggesting that some of these historical case reports should be regarded with caution, as suspected by Rosenbaum and colleagues (53). Furthermore, as suspected by clinical description in some cases, consciousness could have been impaired, precluding any investigation of ictal language properties (17). In more recent years, further report of Wernicke ictal aphasia has been published, with aphasic symptoms lasting as long as 5 and 10 days in a middle-aged woman (55). It is supposed that aphasia occurs when the ictal discharge involves any part of the speech network (31; 43; 59; 01; 34; 44). Aphasic seizures have been reported in multiple sclerosis (57).
Aphasic seizures can eventually evolve to bilateral tonic-clonic seizures or focal status.
Case 1. A 14-year-old boy was first suspected by physicians to have reading epilepsy, because difficulties appeared very often when he was engaged in reading activities. However, video-EEG monitoring showed that spontaneous left temporal lobe seizures could be recorded independent of reading activities. The seizures were characterized by pronounced language difficulties, including ictal paraphasia and difficulties in understanding verbal orders. The Brain MRI showed a left temporal lobe cavernoma, which was then surgically removed. At six months follow-up post-surgery, under antiepileptic drugs, no further seizures were reported.
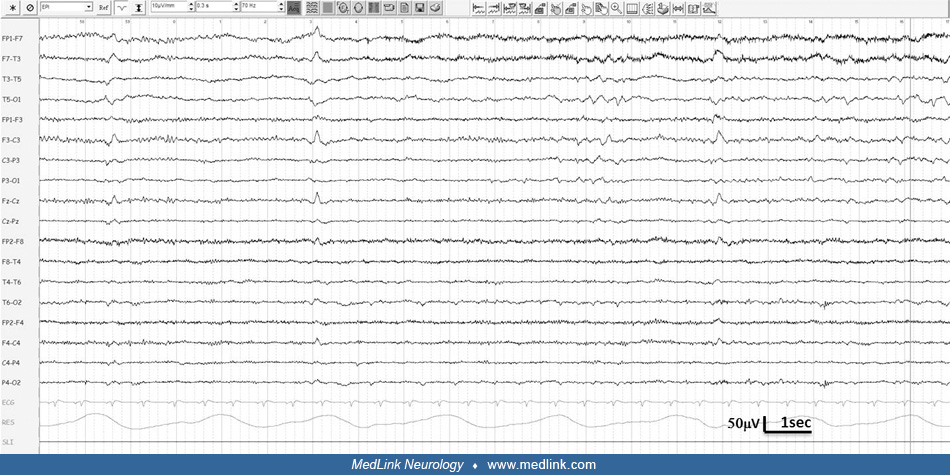
Case 2. A 53-year-old woman with primary brain tumor was treated with levetiracetam since diagnosis one year before. One week before admission, levetiracetam was withdrawn abruptly because no overt seizure was evidenced. During the following days, she presented isolated severe aphasia, with fluent jargon and altered comprehension. She was recorded with video-EEG during her stay in the emergency unit. A continuous rhythmic sharp-wave activity was recorded over the left hemisphere, as the patient showed jargon aphasia while denominating pictures. No change in her brain lesion could be evidenced by imagery, and aphasic status was diagnosed. After 4 mg of lorazepam intravenous infusion during the recording, the EEG improved, but aphasia remained until one day later.
Anatomic correlates of aphasia have been the subject of a great many studies since the first work of Paul Broca, in strong contrast to what is currently known about the brain networks whose epilepsy-related dysfunction may cause ictal aphasia. Since the famous work of Penfield and Jasper, it is well-known that cortical stimulation performed on various sites of the brain could produce either abnormal vocalizations or a transient inability to speak or adequately use words (05). In other intracranial studies, Broca and Wernicke areas and the basal temporal area have been shown to be involved during aphasic seizures or to promote language disturbances when electrically stimulated (34; 56). In a subdural EEG recording and stimulation study in one patient, speech arrest at seizure onset was shown to be related to seizure discharge in the basotemporal region (01). In a study of 172 patients with temporal lobe seizure, 15 (8.7%) patients had seizures caused by temporopolar or anterior temporobasal lesions, with aphasia as the most prominent ictal feature when the lesion was left-sided (61). It remains unknown, however, to what extent the topography of the lesion is relevant for deciphering the ictal symptomatogenic network.
Postictal aphasia remains a frequent complication of dominant hemisphere temporal lobe seizures (02). The value of postictal symptoms has been emphasized, especially in correctly lateralizing the epileptogenic focus. Moreover, in refractory epilepsy amenable to epilepsy surgery, the presence of postictal aphasia could represent an argument to promote further study, including functional imaging, Wada test, or depth electrode recordings to rule out any functional risk during surgery.
The etiologies underlying ictal language disturbances are varied, with inflammatory and vascular lesions being the most frequently detected lesions (63; 29). However, a large study showed that the majority of patients do not have a clear structural lesion (50), and some may be familial, with or without detected gene mutations. The most common mutation in epilepsy with auditory features is in the LGI1 gene, but mutations have been described less frequently in RELN, DEPDC5, MICAL-1, CNTNAP2, and SCN1A genes (07; 47; 12; 22).
Brain imaging techniques can help in showing DWI changes involving specific areas during aphasic status epilepticus (62). Cortical hyperintensity was shown in six of eight patients, mostly in the left temporal-parietal cortex. In this case series, four patients also exhibited thalamic, namely pulvinar, signal changes.
Suspension of ongoing speech often occurs during epileptic seizures. However, in most cases, it relates to an altered state of consciousness, namely loss of contact, making the patient unable to purposefully interact with his environment, either verbally or not. Such patients are not truly aphasic but dont use language because their awareness is impaired.
Another challenging task is to correctly distinguish between isolated mutism and aphasic seizures. Mutism is represented by a refusal to speak although the mechanism of speech is not damaged. In ictal mutism the patient is denying any verbal relationship with relatives or caregivers during the seizure.
During the seizure, loss of contact or mutism may make the patient unresponsive to oral questioning, but not aphasic, so aphasic seizure should be strictly defined as an isolated aphasia during ictal discharge (05). It is self-explanatory that, according to this point of view, each patient should be examined during the seizure with the careful aim to test possible aphasia and to rule out mutism or loss of contact.
In the current literature, distinction between loss of contact, mutism, or true aphasia during a seizure is not always clear. Indeed, the more carefully documented cases are prolonged seizures or status epilepticus, namely nonconvulsive focal status with aphasia, which allowed timely clinical assessment of the speech disorder. It can be presumed that pure aphasic seizures are underestimated, given the difficulties to demonstrate, in the short time of the seizure course, that the patient presented with aphasia and not mutism or loss of contact. The need for specific clinical criteria has been pointed out by several studies, and it has already been discussed in the Clinical manifestations section.
Migraine with prolonged aphasic aura is a differential diagnosis of aphasic seizures, and it is usually associated with hemiplegia in the context of familial hemiplegic migraine (54); however, although rare, aphasia without hemiparesis may occur in migraines associated with channelopathies (30).
Epilepsy with auditory features is a focal epileptic syndrome with onset at variable age (22). It is characterized by seizures with auditory aura or receptive aphasia, suggesting a lateral temporal lobe involvement of the epileptic discharge (22). The etiology is diverse, with some patients having structural lesions on MRI and others with negative MRI with or without family history of epilepsy (47). In autosomal dominant temporal lobe epilepsy with auditory features or familial lateral temporal lobe epilepsy (36), aphasic seizures represent the ictal hallmark of the disease. In such cases, sensory aphasia appears to be the common type of seizure, with a severe comprehension deficit (08), linked to mutations in the LGI1 gene (leucine-rich, glioma inactivated) (25). Familial aphasic episodes should be indicative for the disorder (32). However, in contrast to an auditory aura present in 55% of affected family members, aphasic seizures were not reported among 11 patients (67). In autosomal dominant lateral temporal lobe epilepsy, the aphasic symptoms are transitory and mostly restricted to the ictal phase. The combination of long-lasting aphasia and epileptic seizures is characteristic for Landau-Kleffner syndrome (37; 15; 64), a condition now linked to GRIN2A mutations (09; 38; 39).
These disorders affect young children with previously normal psychomotor development, causing profound regression with loss of receptive and expressive language capabilities (15). The seizures usually remit in adolescence; however, most patients show persistent language dysfunction. However, although language is crucially involved in Landau-Kleffner syndrome, patients do not present with aphasic seizures.
EEG recording of aphasic seizures remains the gold standard for diagnosis. However, in many cases, evidence of interictal discharges on EEG should constitute a valuable argument toward diagnosis and should promote adequate treatment when clinical findings are suggestive (61).
MRI is essential in diagnosing structural lesions that cause seizures and epilepsy (06). However, MRI may reveal transitory changes that are the consequence of seizures rather than its cause (11). Ictal activity during aphasic seizures and aphasic status epilepticus can induce a wide spectrum of MRI brain abnormalities that may be transient (62; 40; 11; 42; 63).
EEG changes in aphasic seizures usually co-localize with MRI and FDG-PET findings (63), but MRI DWI changes may involve subcortical structures, such as the thalamus, in addition to the cortical language areas (62).
Other functional imaging techniques like ictal SPECT or CT perfusion may show abnormal perfusion patterns involving language areas (41), and interictal FDG-PET could reveal focal hypometabolism. Language tasks-correlated fMRI provides valuable information regarding hemispheric dominance for verbal functions (18; 63). With respect to aphasic seizures, such exploration may be of substantial help in matching presumed epileptogenic zone and language areas.
Antiseizure medications are required as usual. In specific cases, etiologic treatment can also apply.
In cases of nonconvulsive status epilepticus, physicians should be cautious not to cause additional harm by promoting invasive therapy, such as orotracheal intubation due to sedative antiseizure medication use, as aphasic status has been shown to last up to several days, with language recovery exceeding EEG improvement by hours to days (19).
All contributors' financial relationships have been reviewed and mitigated to ensure that this and every other article is free from commercial bias.

Fernando Cendes MD PhD
Dr. Cendes of the University of Campinas - UNICAMP has no relevant financial relationships to disclose.
See Profile
Jerome Engel Jr MD PhD
Dr. Engel of the David Geffen School of Medicine at the University of California, Los Angeles, has no relevant financial relationships to disclose.
See ProfileNearly 3,000 illustrations, including video clips of neurologic disorders.
Every article is reviewed by our esteemed Editorial Board for accuracy and currency.
Full spectrum of neurology in 1,200 comprehensive articles.
Listen to MedLink on the go with Audio versions of each article.
MedLink®, LLC
3525 Del Mar Heights Rd, Ste 304
San Diego, CA 92130-2122
Toll Free (U.S. + Canada): 800-452-2400
US Number: +1-619-640-4660
Support: service@medlink.com
Editor: editor@medlink.com
ISSN: 2831-9125
Epilepsy & Seizures
Jul. 19, 2024
Epilepsy & Seizures
May. 27, 2024
Neuroimmunology
May. 24, 2024
Epilepsy & Seizures
May. 22, 2024
General Child Neurology
May. 15, 2024
Epilepsy & Seizures
May. 10, 2024
Epilepsy & Seizures
Apr. 29, 2024
Epilepsy & Seizures
Apr. 22, 2024