Neurobehavioral & Cognitive Disorders
Transient global amnesia
Jul. 19, 2024
MedLink®, LLC
3525 Del Mar Heights Rd, Ste 304
San Diego, CA 92130-2122
Toll Free (U.S. + Canada): 800-452-2400
US Number: +1-619-640-4660
Support: service@medlink.com
Editor: editor@medlink.com
ISSN: 2831-9125
Toll Free (U.S. + Canada): 800-452-2400
US Number: +1-619-640-4660
Support: service@medlink.com
Editor: editor@medlink.com
ISSN: 2831-9125
Worddefinition
At vero eos et accusamus et iusto odio dignissimos ducimus qui blanditiis praesentium voluptatum deleniti atque corrupti quos dolores et quas.
After carpal tunnel syndrome, the most common median nerve entrapment is the pronator teres syndrome (04). Other less common entrapment sites include the ligament of Struthers, lacertus fibrosus, and the tendinous origin of the flexor digitorum superficialis.
In 1848, Struthers depicted in finer detail the supracondylar process 5 cm above the medial epicondyle and its ligament. Struthers ligament can compress the median nerve (12). Anterior interosseous neuropathy was originally described in two patients who had spontaneous recovery (09). Around the same time, the pronator teres syndrome was recognized (24). Median nerve entrapment under the bicipital aponeurosis was described over two decades ago (11).
The most common features of the pronator teres syndrome are insidious proximal forearm fatigability, pain, and tenderness amplified by exercise and at times radiating to the shoulder (14). Slight objective muscle weakness is frequently detectable, involving median-innervated forearm (possibly including pronator teres muscle) and hand muscles, especially the flexor pollicis longus. Most cases develop thumb and index numbness that are exacerbated by resisted pronation. Sensory findings are vague. Nocturnal pain or paresthesia is unusual and lends support to the much more common carpal tunnel syndrome. Tinel sign may be positive at the forearm. Pressure on the pronator teres may reveal firmness or cause pain radiation. We have observed the pronator teres syndrome in association with forearm dystonia after stroke.
Median nerve entrapment rarely occurs at the ligament of Struthers or supracondylar spur. Despite vague clinical presentation, features include associated brachial artery claudication, radial pulse attenuation and exacerbation of pain and numbness by resisted elbow extension with forearm supination, and palpable or radiographically visible supracondylar spur (22). The spur can be a few millimeters to 20 mm long. It occasionally also compresses the ulnar nerve (08).
Median nerve compression at the bicipital aponeurosis most commonly manifests acutely with forearm and elbow pain (16). Most patients have forearm Tinel sign and weakness that may involve the pronator teres muscle. Forearm pain and hand paresthesias are augmented by resisted elbow flexion (22). Sensory symptoms are not ubiquitous.
The anterior interosseous nerve branches 5 to 8 cm distal to the elbow. Weakness in the anterior interosseous syndrome affects one or more of the following muscles: flexor pollicis longus, flexor digitorum profundus I, flexor digitorum profundus II, and pronator quadratus. On attempting to form a circle with the index and thumb, metacarpophalangeal and proximal phalangeal hyperflexion compensates for distal phalangeal joint hyperextension: the so-called pinch sign. The flexor digitorum profundus to the index is more commonly affected than that to the middle finger. Partial lesion usually results in selective weakness of the flexor pollicis longus. Pain and tenderness in the wrist or elbow are variable but in classic nontraumatic cases antedate weakness. Pain is exacerbated by resisted proximal interphalangeal flexion of the middle finger (22). Tapping on the nerve may provoke pain radiating to the wrist.
Additional causes of median neuropathy in the forearm include ischemia, mass lesions, and electrical burns (22). Ischemic monomelic neuropathy following arteriovenous fistula placement sometimes can predominantly affect the median nerve. Mononeuritis multiplex affects the median nerve in almost half of the cases. Forearm blunt trauma can increase compartment pressure resulting in muscle and nerve injury. Antecubital venous puncture in the anticoagulated patient poses risk for hematoma that might require emergent decompression. Thrombophlebitis of the median basilic vein can compress the median nerve at the antecubital space.
In a tertiary care center population, we identify on the average four patients with median neuropathy at the forearm for every 100 carpal tunnel syndrome patients. These are predominantly attributed to penetrating trauma to the upper forearm or elbow and perioperative compression.
Peperkamp and colleagues reviewed adult cases of published median nerve compression since 2000 thought to be due to anatomical structures (20). Out of 74 cases, the most common compression site was the carpal tunnel, with only 18 being located more proximally at the arm or forearm. The most commonly observed anatomic etiologies were isolated and consisted of muscular compression, vascular causes, or anomalous nerve course. Less common etiologies occurred as a combination of these findings.
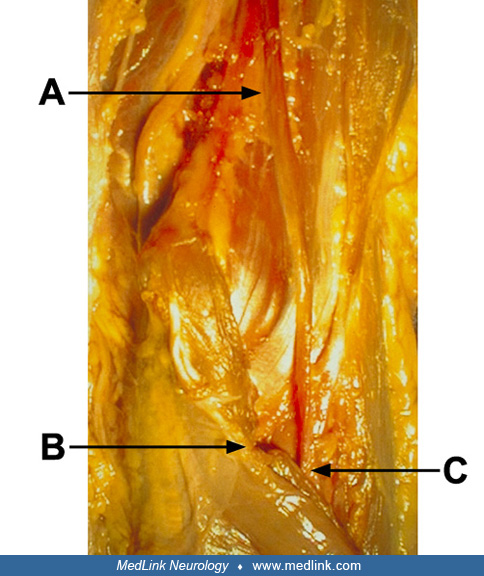
A 34-year-old man was treated at a hospital for a stab wound 3 cm above the left medial epicondyle. He complained of persistent left forearm and hand numbness and of being unable to pinch with his index and thumb. On physical examination 2 months after injury, he had partial sensory loss in the left medial forearm and complete sensory loss in the left hand median distribution and thenar eminence. He could elevate his thumb to 30 degrees without resistance. He was unable to pronate his forearm. Forearm flexor compartment was severely atrophied. Tinel sign elicited on scar percussion was reportedly nonadvancing. On nerve conduction studies his left median sensory and motor responses were absent. Severe active denervation without motor units was evident in the left abductor pollicis brevis, opponens pollicis, pronator teres, flexor digitorum superficialis, median head of flexor digitorum profundus, and flexor pollicis longus. He subsequently underwent surgical exploration of his left median nerve at the elbow.
In the literature, causes of the pronator teres syndrome are variable. On surgical exploration, compression by the pronator teres, lacertus fibrosus, or tendinous origin of the flexor digitorum superficialis were almost uniformly demonstrated (07). Others argue that these anomalies are quite common in the general population (26). Although focal median nerve entrapment may occur, most anterior interosseous neuropathies are felt to be immune-mediated. Evidence of localized nerve compression by the ligament of Struthers is usually only surgically available (08). Entrapment at the bicipital aponeurosis is both surgically and electrophysiologically demonstrable (16).
Pronator teres syndrome may be associated with an enlarged or anomalous origin of pronator teres, hypertrophied bicipital aponeurosis, fibrous band within the muscle, taut tendinous origin of the flexor digitorum superficialis, accessory origin of flexor carpi radialis, persistent median artery, or increased forearm compartment pressure. Median and ulnar nerve damage at the proximal forearm with distal Colles fracture has been reported and ascribed to stretch tension (23).
Nerve inflammation has been implicated as the main cause of anterior interosseous neuropathy based on frequently normal operative findings and spontaneous improvement without surgery (26). Although the nerve can be chronically compressed by the edge of the flexor digitorum sublimis, deep head of pronator teres, or accessory head of the flexor pollicis longus these anatomic variants are common in asymptomatic individuals. Furthermore, neuralgic amyotrophy may be associated with contralateral or ipsilateral anterior interosseous neuropathy (19). In order to identify the lesion site in anterior interosseous neuropathy, high-resolution magnetic resonance neurography of the median nerve in the arm and forearm was performed on 20 patients and 20 matched controls (21). Selective T2 lesions in median nerve fascicles destined to be part of the anterior interosseous nerve were detected within the upper arm median nerve trunk in all anterior interosseous neuropathy cases but not in controls. Most lesions were located 14.6 ± 5.4 cm proximal to the humeroradial elbow joint, and these were multifocal in 17 out of 20 cases. This lends further support to the concept that anterior interosseous is a forme fruste of neuralgic amyotrophy. A less frequent cause of anterior interosseous compromise is acute direct trauma: supracondylar humeral fracture in children, posterior dislocation of the elbow, forearm fractures, forearm trauma, occlusion of the anterior interosseous artery, or iatrogenic external compression.
Although ligament of Struthers and supracondylar process affect 2% of the population, most are asymptomatic (26). In very few patients these structures will visibly compress the median nerve (08). When tight or thickened, the lacertus fibrosus may flatten an edematous median nerve (16).
In 238 consecutive patients, median neuropathy was proximal to the carpal tunnel in 11% (04). Most were diagnosed with the pronator teres syndrome (9%). Evaluating 101 carpal tunnel syndrome cases, others reported pronator teres syndrome in seven patients (14). Our experience suggests that these may be overestimates. Patients with genetic predisposition for pressure palsy are at increased risk (03). Repetitive forceful elbow pronation and flexion renders individuals more prone to nerve compression syndromes at the elbow.
Avoidance of repetitive forearm pronation and elbow flexion may prevent hypertrophy of the pronator teres muscle. This, in turn, would reduce the likelihood of median or anterior interosseous nerve compromise.
Median neuropathy at the forearm should not be confused with carpal tunnel syndrome, brachial plexopathy, cervical radiculopathy, or median neuropathy in the axilla, upper arm, or distal to the carpal tunnel. A case of small cortical stroke in the “hand knob” was associated with marked weakness of the thumb and index flexion, mimicking an anterior interosseous neuropathy (05).
Carpal tunnel syndrome is more frequently a cause of forearm pain. Evidence in support of carpal tunnel syndrome includes nocturnal or rest-induced paresthesias, digital sensory loss and weakness limited to the abductor pollicis brevis, opponens pollicis, and lumbricalis. Features in forearm entrapment are persistent pain without diurnal variation, focal forearm tenderness, and weak forearm muscles.
Lateral cord neuralgic amyotrophy at times mimics median neuropathy.
Cervical radiculopathy can result in forearm pain exacerbated by neck movements. Compression of the sixth or seventh cervical roots is accompanied by neck pain, paresthesias of the thumb, index, or middle finger, reflex asymmetry, and weak shoulder or arm muscles.
Finally, in rheumatoid arthritis, there is a predilection for spontaneous rupture of the tendons of the flexor pollicis longus or index flexor digitorum profundus, or both, due to scaphoid bony spur formation (22). Tendon integrity is demonstrable when thumb and index flex in response to pressure applied radially 5 cm proximal to the wrist.
Median neuropathy in the arm may complicate midhumeral fracture and progress due to callus formation or muscle fibrosis (22). Median nerve and brachial artery transection can spare the ulnar nerve in distal arm laceration. Arm compartment syndrome can compress the median nerve.
Median neuropathy in the axilla is occasionally seen from compression or trauma. Compression is suspected with crutch use, "sleep" palsy, axillary block anesthesia, and axillary arterial cannulation. The later potentially causes an acute combined median and ulnar neuropathy due to medial brachial fascial compartment syndrome (25). Shoulder dislocation or proximal humeral neuropathies are more likely to damage the axillary than median nerve.
Median neuropathy distal to the carpal tunnel is very uncommon. Digital nerve compression may be acute (forced digit hyperextension) or chronic (bowling, scissors, vibrating tools, etc.) Terminal median motor or recurrent thenar branch damage is a result of chronic blunt trauma, ganglion, or arterial compression.
Median nerve compression in the distal forearm is rare and mimics carpal tunnel syndrome. Causes are varied: blunt trauma, distal forearm fracture, or fascial fibrosis in scleroderma (10). The median palmar cutaneous nerve supplying the thenar eminence may be compromised by fascia or ganglion. For a more detailed discussion of median neuropathy in the distal forearm or distal to the carpal tunnel, the reader is referred to Rosenbaum and Oschoa (22).
Flu-like illness may precede severe shoulder and arm pain. Days to weeks later, and as the pain becomes more bearable, weakness rapidly appears and is typically maximal at onset. Of 136 patients, one patient had selective involvement of the anterior interosseous nerve (19). Since then, others have confirmed this observation (09; 13). Careful examination in most patients uncovers additional nonmedian sensory loss and weakness as well as reflex asymmetry.
Like Tinel sign, provocative tests should be cautiously interpreted due to their lack of specificity. Nerve conduction and electromyography are helpful to establish median nerve compromise from entrapment at the elbow. More importantly, the study can rule out carpal tunnel syndrome, neuralgic amyotrophy, and cervical radiculopathy.
Most patients with pronator teres syndrome, however, have normal electrodiagnostic testing (07; 28). In only one series, most patients with pronator teres syndrome (6 out of 7) had median motor slowing at the forearm (14). Three of nine other patients had a 20% or higher drop in motor amplitude recording from the abductor pollicis brevis after resisted pronation with forearm extension (28). These abnormalities reverted following surgical release. Side-to-side comparison of median motor amplitudes recording from the pronator teres may be helpful when that muscle is weak. With unremarkable electrodiagnostic studies there may be a role for dynamic compartment pressure measurements prior to and after exercise (06). In addition to abnormal median innervated forearm muscles, electromyography may occasionally show denervation of the pronator teres due to distal branching. The flexor carpi radialis and flexor digitorum sublimis may be spared due to nerve branching proximally.
Median motor conduction of the pronator quadratus using needle recording electrode demonstrated prolonged latencies in 5 out of 7 anterior interosseous neuropathies (15). This technique is, however, cumbersome. An alternate technique using surface electrodes over the flexor pollicis longus has been reportedly successful in demonstrating reduced motor amplitude and prolonged distal latency (03). These changes normalized with clinical improvement. Again, denervation is restricted to the flexor pollicis longus, pronator quadratus, and flexor digitorum profundus I and II.
There is a spectrum of abnormalities with entrapment at the bicipital aponeurosis (16). Nelson and colleagues reported one and reviewed seven published cases: one patient had no diagnostic abnormalities, nerve conduction studies were localizing in five patients, and denervation of median-innervated muscles were prominent in six patients. In a case report of surgically proven entrapment at ligament of Struthers and a literature review of another thirteen cases, electromyography was nonlocalizing (08).
Various radiological signs have been described in the orthopedic literature to support median nerve entrapment by callus. These include bony canal in the radius (01) and incomplete circular defect 6 weeks after medial epicondylar fracture (18).
On evaluating ultrasonographically median nerve elasticity, researchers reported that the strain ratio of the median nerve/flexor digitorum superficialis muscle was significantly lower in leprosy as compared to a group of healthy volunteers (17).
Hartz and colleagues noticed improvement in only 2 of 7 medically treated pronator teres syndrome cases and one got worse. Another group reported earlier better success after 1 to 2 months of conservative management in 5 out of 7 electrodiagnostically confirmed demyelinating pronator teres syndrome cases (14). Measures include forearm resting and elbow splint, job and hobby modification, topical injection of local anesthetic or steroid, and subsequent physical therapy. Conservative treatment is more successful for idiopathic anterior interosseous syndrome with an 80% or higher recovery rate (15; 13). Depending on severity, surgery is also contemplated after 3 to 6 months for persistent nonprogressive symptoms (02). Progressive symptoms refractory to medical management or neurophysiologic evidence of severe axonal loss dictate earlier surgical exploration exposing the various forearm entrapment sites from the flexor digitorum sublimis to the ligament of Struthers. When gross operative findings are mild, intraoperative segmental median nerve stimulation is useful as an adjunct to confirm the site of abnormality (16). Most surgically treated patients in the Mayo clinic series had either complete or good relief from pronator teres syndrome (07). Failures were felt to be due to misdiagnosis or inadequate release. Improvement is predictable in patients with operatively demonstrable nerve compression. If recovery from severe nerve entrapment is unsatisfactory at 18 to 24 months, tendon transfer needs to be considered to restore thumb and index pincer function.
The management of idiopathic anterior interosseous neuropathy is mainly conservative. In a retrospective analysis of 14 patients, eight who were treated conservatively exhibited spontaneous recovery at 3 to 12 months after onset (27). In six patients who did not show any improvement at 3 months, the nerve was explored and released from compressing structures. At follow up ranging 2 to 9 years after onset, only one patient had poor postoperative outcome necessitating tendon transfer.
Symptomatic entrapment by the ligament of Struthers has good outcome from surgical release and possibly neurolysis (08). All reported cases of median nerve entrapment at the bicipital aponeurosis underwent surgical release with improved pain and strength (16).
Acute forearm compartment syndrome dictates swift fasciotomy. Penetrating forearm or elbow trauma necessitates emergent surgical exploration to assess median nerve integrity.
Median neuropathy in the arm or axilla is best managed medically. However, in the absence of an inciting injury, arteriography or even exploration may be necessary (02).
Caution needs be exerted to avoid extrapolating these recommendations to patients with forearm pain in the absence of either clinical or electrodiagnostic evidence of nerve compromise. This surgical approach is not indicated in managing lateral epicondylitis or pronator teres/forearm muscle strain.
Prognosis is generally good with conservative management of forearm pain in the absence of electrodiagnostic abnormalities. Recovery from spontaneous anterior interosseous syndrome is anticipated as early as 6 weeks to 6 months and is complete at 12 to 18 months. In cases of median conduction block without axon loss refractory to conservative management, complete postoperative recovery is anticipated in the first few weeks to months. Recovery from axonal injury is more delayed and in severe cases functional improvement is incomplete. The lateral antebrachial cutaneous nerve can be inadvertently injured during elbow surgery.
All contributors' financial relationships have been reviewed and mitigated to ensure that this and every other article is free from commercial bias.

Mazen M Dimachkie MD
Dr. Dimachkie, Director of the Neuromuscular Disease Division and Executive Vice Chairman for Research Programs, Department of Neurology, The University of Kansas Medical Center received consultant honorariums from Abata/Third Rock, Abcuro, Amicus, ArgenX, Astellas, Cabaletta Bio, Catalyst, CNSA, Covance/LabCorp, CSL Behring, Dianthus, EMD Serono/Merck, Horizon, Ig Society Inc, Ipsen, Janssen, Octapharma, Priovant, Ra Pharma/UCB Biopharma, Sanofi Genzyme, Shire/Takeda, Treat NMD/TACT, and Valenza Bio. Dr. Dimachikie also received research grants from Alexion/Astra Zaneca, Amicus, Astellas, Catalyst, CSL Behring, EMD Serono/Merck, Genentech, Grifols, GSK, Horizon, Janssen, Mitsubishi Tanabe Pharma, MT Pharma, Novartis, Octapharma, Priovant, Ra Pharma/UCB Biopharma, Sanofi Genzyme, Sarepta Therapeutics, Shire/Takeda, and TMA.
See Profile
Francine J Vriesendorp MD
Dr. Vriesendorp of SUNY Upstate Medical University in New York has no relevant financial relationships to disclose.
See Profile
Randolph W Evans MD
Dr. Evans of Baylor College of Medicine received honorariums from Abbvie, Amgen, Biohaven, Impel, Lilly, and Teva for speaking engagements.
See ProfileNearly 3,000 illustrations, including video clips of neurologic disorders.
Every article is reviewed by our esteemed Editorial Board for accuracy and currency.
Full spectrum of neurology in 1,200 comprehensive articles.
Listen to MedLink on the go with Audio versions of each article.
MedLink®, LLC
3525 Del Mar Heights Rd, Ste 304
San Diego, CA 92130-2122
Toll Free (U.S. + Canada): 800-452-2400
US Number: +1-619-640-4660
Support: service@medlink.com
Editor: editor@medlink.com
ISSN: 2831-9125
Neurobehavioral & Cognitive Disorders
Jul. 19, 2024
Peripheral Neuropathies
Jul. 17, 2024
Neuro-Ophthalmology & Neuro-Otology
Jul. 17, 2024
Neuro-Ophthalmology & Neuro-Otology
Jul. 17, 2024
General Neurology
Jul. 11, 2024
Headache & Pain
Jul. 06, 2024
Neuro-Ophthalmology & Neuro-Otology
Jun. 21, 2024
Neuro-Ophthalmology & Neuro-Otology
Jun. 18, 2024